Introduction
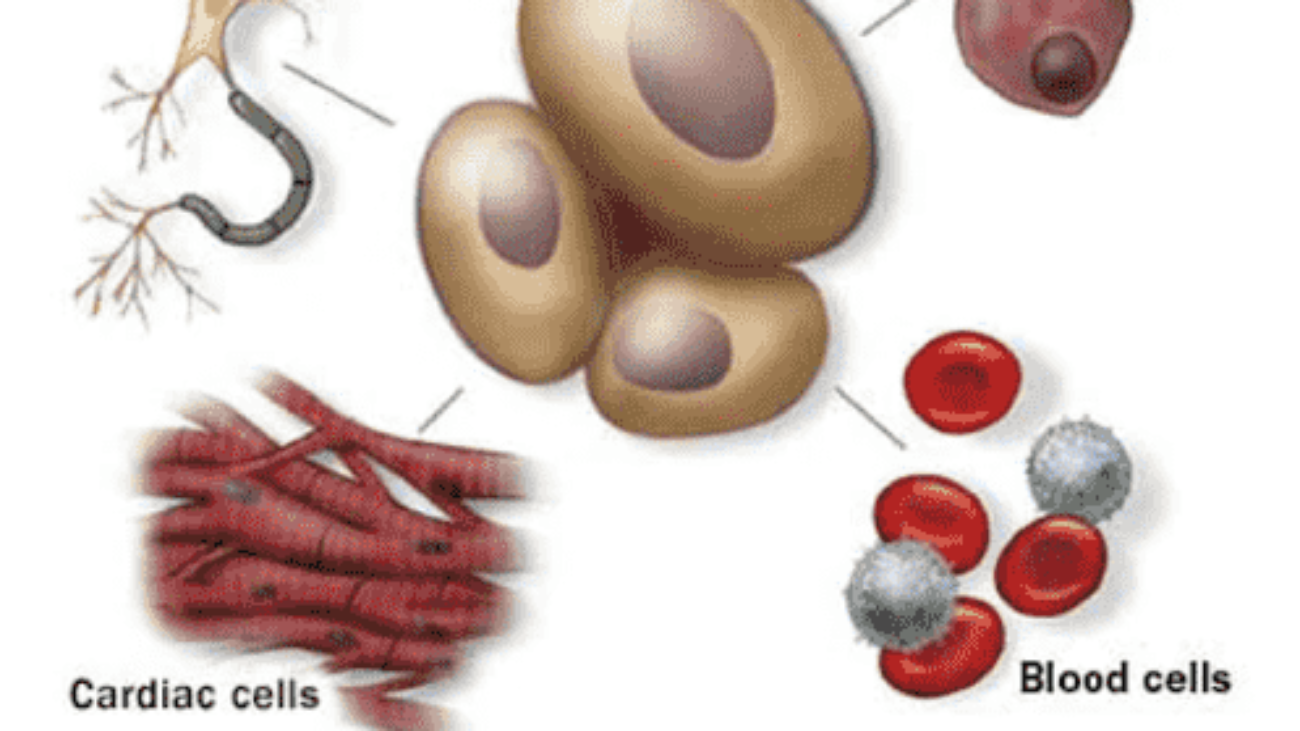
Probiotics–defined as live microorganisms that offer health benefits–have gained significant attention for their potential to improve gut health and support the immune system. These beneficial bacteria are primarily found in fermented foods and supplements, playing a crucial role in maintaining balance within the gut microbiota. In other words, they can impact the immune system’s function. The intricate relationship between the gut and the immune system is crucial, as around 70% of the body’s lymphocytes (a type of white blood cells crucial for the immune system) reside in the gastrointestinal tract. Although many studies show their beneficial effects on the human body, there is a lack of definitive evidence supporting the benefits of specific strains of bacteria or probiotic dosages. As a result, this article will discuss the effects of probiotics on the immune system, highlighting their role in reducing the risk of infections, allergies, and autoimmune conditions.
Gut Microbiota
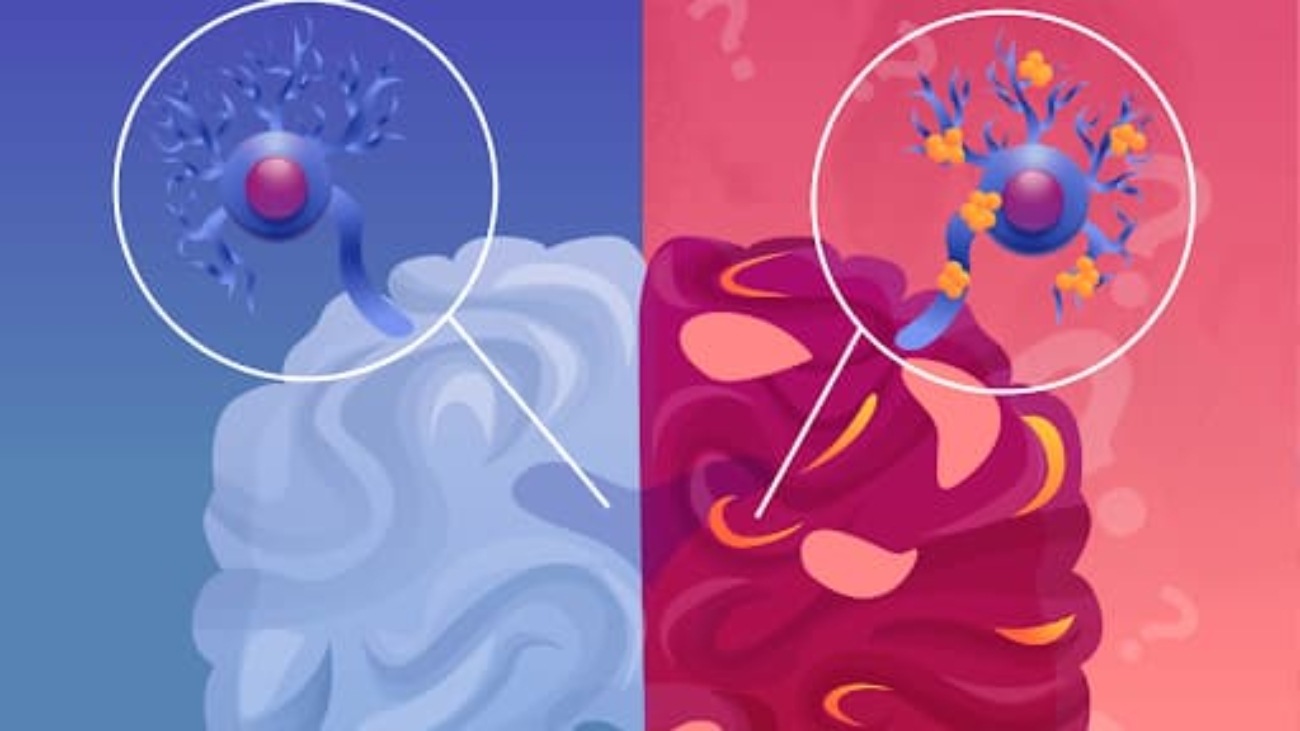
The gut microbiota is a system of trillions of microorganisms within the human gastrointestinal tract. This system contains bacteria, fungi, and viruses, with bacteria being particularly influential on health. The gut microbiota plays a crucial role in interacting with the innate and adaptive immune system, maintaining homeostasis and preventing inflammation. It helps with digestion, vitamin production, protection against harmful pathogens, and the creation of fatty acids that facilitate communication between the gut and immune cells. The gut epithelial cells form a mucosal barrier to separate the microbiota and the immune cells to prevent harmful substances from entering the bloodstream. If the interaction between gut bacteria and the immune system is disrupted, harmful bacteria called “Gram-negative bacteria” grow and damage the mucosal barrier, leading to infections and increased intestinal permeability.
Additionally, when the gut microbiota becomes imbalanced (gut dysbiosis) with increased harmful bacteria, it negatively impacts the immune system, causing inflammation, oxidative stress, and insulin resistance. Gut dysbiosis is caused by various factors, including the use of antibiotics and antimicrobial agents, drugs, smoking and alcohol, physical and psychological stress, chronic inflammation, and an unbalanced diet. Over time, chronic dysbiosis can lead to long-term conditions such as type 2 diabetes, cardiovascular diseases, inflammatory bowel diseases, autoimmune disorders, and certain cancers. Probiotics play a significant role in the gut microbiota composition, which can inhibit the growth of harmful bacteria in the gastrointestinal tract. As a result, it helps the host build a healthy intestinal mucosa protective layer, decrease permeability, and enhance the immune system.
How probiotics interact with the immune system
Probiotics can strengthen the gut barrier, preventing harmful pathogens from entering. They interact with special immune cells in the gastrointestinal tract, such as dendritic cells, macrophages, and T and B lymphocytes. They also interact with the host’s intestinal cells at the surface of the intestinal barrier, including the intestinal epithelium and underlying lamina propria.
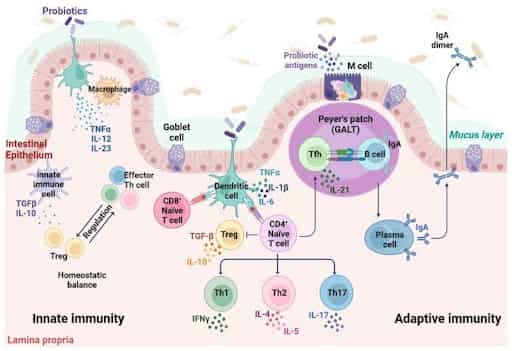
When consuming food with probiotics, they adhere to intestinal epithelial cells and send signals to the immune cells by Pattern Recognition Receptors (PRRs). Cytokines, which are stimulated by probiotic bacteria, activate T-regulatory (Treg) cells, maintaining immune homeostasis in the intestinal mucosa. Treg cells help suppress a strong immune response, which could lead to problems such as allergies (where there is a strong immune response to harmless substances causing allergic reactions). There are specialized enterocytes (specialized cells that line the inner surface of the small intestine and play a crucial role in nutrient absorption) called “Microfold cells” (M cells), which act as messengers and transporters, passing information about harmful bacteria to immune cells and transferring intestinal antigens to dendritic cells. Depending on the situation, the intestinal Dendritic cells activate Th1, Th2, or Th17 immune responses.
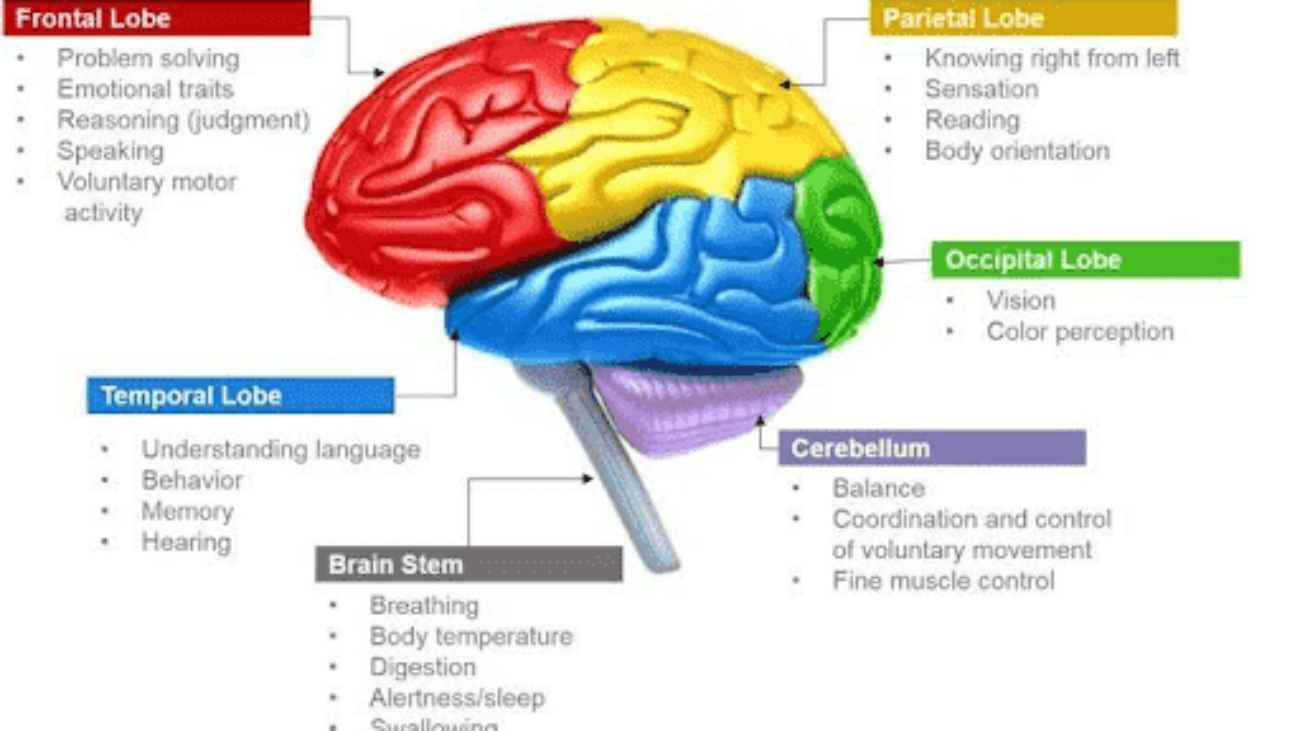
Th1 immune response is responsible for fighting intracellular pathogens such as viruses and bacteria, activating macrophages to kill infected cells.
Th2 defends against extracellular parasites and handles allergies, activating B cells to produce antibodies (IgE) for defense.
Th17 targets extracellular bacteria and fungi, activating neutrophils (the most abundant type of white blood cell in the innate immune system) to increase inflammation and fight infection.
Additionally, probiotics induce the maturation of B cells, to create IgA antibodies, which then produce plasma cells that stick to germs to present bacterial adhesion to the host’s tissues.
Benefits of Probiotics on Immune and Human Health
Probiotics are mainly Gram-positive bacteria, including species belonging to the Lactobacillus and Bifidobacterium genre, such as Escherichia coli, Enterococcus, Pediococcus, and Yeast species. They have several beneficial effects, such as ameliorating innate immune responses and related anti-pathogenic/inflammatory activities, improving the absorption of beneficial nutrients, and decreasing food intolerance.
They also inhibit the growth of pathogenic bacteria by synthesizing compounds with low molecular weight, such as acetic and lactic acids and “bacteriocins, ” which are antimicrobial compounds with large molecular weights. Bacteriocins produced by probiotics include lactacin B from L. acidophilus, Bifidocin B from Bifidobacterium bifidum NCFB, plantaricin from L. plantarum, and nisin from Lactococcus lactis. These compounds have shown inhibitory effects against Gram-negative pathogens, such as H.pylori.
The gut barrier is essential for separating the gut bacteria and the body. Mucus is a secretory immunoglobulin A (sIgA), an antibody that plays a critical role in the immune system at the mucosal sites. The sIgA produces plasma cells in the intestinal tissues and transports antibodies across the intestinal epithelial cells into the gut lumen. The antibody binds to pathogens and toxins, preventing them from causing harm through immune exclusion, a non-inflammatory response. Probiotics have been shown to increase the number of sIgA-producing cells in the gut and other mucosal areas, such as the bronchus and mammary glands, exhibiting how probiotics can enhance the immune response by prompting the production of sIgA.
Conclusion
Probiotics play a critical role in modulating the gut microbiota, positively impacting the immune system. Their interactions with various immune cells help maintain immune homeostasis, strengthen gut barriers, and enhance the body’s ability to fight against infections, allergies, and autoimmune disorders. Although the effectiveness of specific probiotic strains and optimal dosages are still being researched, current evidence demonstrates their ability to support innate and adaptive immunity. A deeper understanding of the gut-immune relationship can contribute to multi-faceted approaches involving probiotics, which have considerable promise in preventing immune disorders, potentially enabling more targeted therapeutic applications.
Sources:
Cleveland Clinic. (2024, April 16). What Is Gut Dysbiosis? Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/dysbiosis
Gourbeyre, P., Denery, S., & Bodinier, M. (2011). Probiotics, prebiotics, and synbiotics: impact on the gut immune system and allergic reactions. Journal of Leukocyte Biology, 89(5), 685–695. https://doi.org/10.1189/jlb.1109753
Liu, Y., Wang, J., & Wu, C. (2022). Modulation of Gut Microbiota and Immune System by Probiotics, Pre-biotics, and Post-biotics. Frontiers in Nutrition, 8. https://doi.org/10.3389/fnut.2021.634897
Maldonado Galdeano, C., Cazorla, S., Lemme Dumit, J., Vélez, E., & Perdigón, G. (2019). Beneficial Effects of Probiotic Consumption on the Immune System. Annals of Nutrition and Metabolism, 74(2), 115–124. https://doi.org/10.1159/000496426
Mazziotta, C., Tognon, M., Martini, F., Torreggiani, E., & Rotondo, J. C. (2023). Probiotics Mechanism of Action on Immune Cells and Beneficial Effects on Human Health. Cells, 12(1), 184. https://doi.org/10.3390/cells12010184
Wang, X., Zhang, P., & Zhang, X. (2021). Probiotics Regulate Gut Microbiota: An Effective Method to Improve Immunity. Molecules, 26(19), 6076. https://doi.org/10.3390/molecules26196076
Yoo, J., Groer, M., Dutra, S., Sarkar, A., & McSkimming, D. (2020). Gut Microbiota and Immune System Interactions. Microorganisms, 8(10), 1587. https://doi.org/10.3390/microorganisms8101587 (Figure 1)